Thursday, September 30, 2021
Senior Sex
Category: Diseases and Conditions
Created: 3/7/2002 12:00:00 AM
Last Editorial Review: 9/29/2021 12:00:00 AM
* This article was originally published here
Wednesday, September 29, 2021
Q and A: Reducing the risk of medication errors

DEAR MAYO CLINIC: My friend's father recently died from a medication error. One of his prescriptions was filled incorrectly and caused a fatal reaction. I take multiple medications for various conditions. How can I reduce my risk for a medication error?
* This article was originally published here
Tuesday, September 28, 2021
‘SOFA’ triage protocol disadvantages Black COVID patients

A patient assessment protocol called SOFA, or sequential organ failure assessment, may disadvantage Black patients seeking emergency room care for COVID-19, research finds.
During the worst of the COVID-19 pandemic, overwhelmed doctors and nurses in some places have had to make agonizing decisions about which patients should receive scarce health care resources. Some hospitals have contemplated using a standard measurement to guide these decisions. But two new studies in the journal PLOS ONE suggest that SOFA could promote racial disparities in treatment outcomes.
Developed two decades ago to assess illness severity among patients with sepsis, SOFA was designed to help predict which patients have the best chances of survival. A patient with a high SOFA score, according to the protocol, has a lower chance for survival.
In one of the new studies, researchers find that Black patients with COVID-19 admitted to Yale New Haven Health System hospitals typically have higher SOFA scores than white patients do.
The other study shows that while Black patients admitted in the Yale New Haven Health System tended to have higher SOFA scores than those of other racial or ethnic groups, their mortality rate was about the same.
“If we adopt this protocol [SOFA], we could end up disproportionally steering resources away from Black patients and towards other groups,” says Benjamin Tolchin, director of Yale New Haven Health’s Center for Clinical Ethics, and corresponding author of the second paper.
The Yale New Haven Health System is not using SOFA to guide patient care or inform allocation of resources. But other US hospitals have used the scores as a tool for rationing care during the recent surge in COVID-19 cases.
Since the earliest days of the pandemic, some health facilities have been forced to triage patients based on limited supplies. During the first wave of infections in the spring of 2020, some hospitals in northern Italy and New York City lacked the staff and equipment—such as ventilators and hemodialysis machines—needed to assist all emergency cases.
“What happened was that clinicians were making resource allocations decisions on a case-by-case basis, with some preference given to younger patients who were less likely to die from severe infection,” Tolchin says.
While some hospitals began contemplating the use of crisis standard protocols—including those that rely on criteria such as SOFA scores—these protocols had not been used until recently. In Idaho late this summer, for example, physicians were forced to ration medical care in response to the latest local surge in infections, adopting SOFA scores to guide these decisions.
Developed in 1996, the SOFA system calculates the mortality of patients based on the function of six organ systems.
“When we looked at this earlier this year, we were thinking of devising crisis standard of care recommendations that might be adopted in future pandemics,” Tolchin says. “We didn’t think we would be needing them so quickly.”
Source: Yale University
The post ‘SOFA’ triage protocol disadvantages Black COVID patients appeared first on Futurity.
* This article was originally published here
Monday, September 27, 2021
Tens of thousands of New York health care workers could lose jobs as soon as today over vaccine

Tens of thousands of health care workers across New York state could lose their jobs as soon as today, the state-imposed deadline for them to receive the COVID-19 vaccine.
* This article was originally published here
Sunday, September 26, 2021
Saturday, September 25, 2021
New COVID-19 Restrictions Are Making Unvaccinated People More and More Isolated

- People who have refused to get vaccinated against COVID-19 are now facing more restrictions at jobs, entertainment venues, sporting events, and restaurants.
- The unvaccinated say the growing limitations make them feel isolated and targeted.
- Experts say it’s important to understand the feelings of the unvaccinated, but add that restrictions are necessary to combat the COVID-19 pandemic.
Are we creating a two-tiered COVID-19 society?
Those on the non-vaccinated side of pandemic restrictions say it certainly feels that way.
On the other hand, government and business officials who are implementing the restrictions for health and safety reasons say they have no other choice.
Meanwhile, sociology experts say non-vaccinated people, rather than simply swayed by politics, may have been influenced by a combination of societal health shifts that began in the 1980s and by a seemingly endless modern day flow of misinformation.
One sociologist calls them “victims” but with an addendum.
“I think it’s very easy to blow off those who have chosen to be anti-vax as [uneducated, stubborn, and political],” Richard Carpiano, PhD, MPH, a professor of public policy at the University of California Riverside, told Healthline.
“But these are people who are victims. Misinformation has been circulated at almost a faster pace than the virus itself, and these people may have fallen victim to that,” he explained.
There are also some people, he added, who still have trouble accessing the vaccine or who have legitimate reasons to not be vaccinated.
The addendum? The restrictions are needed.
“You do have a choice [whether to get vaccinated],” Carpiano said. “We’ve done the carrots and they are important, but unfortunately now we have to do more.”
What the unvaccinated face
Restrictions on what unvaccinated people can do and what they must do to take part in activities — from dining to enjoying a sports team to going to work — are popping up on both local and national levels.
At TD Garden in Boston, the home of the Celtics and Bruins as well as the setting for concerts and other events, all attendees over the age of 12 will be required to show proof of vaccination or a negative COVID-19 test (at-home tests are not accepted) as of September 30.
In San Francisco, vaccine proof is now required to enter restaurants, bars, large indoor events, and fitness centers.
Large businesses, such as Facebook and Google, are requiring vaccines or regular testing (at the employee’s expense). More businesses are following suit.
Los Angeles County put strict requirements into place as well, and could add more should things not improve, Dr. Muntu Davis, MPH, Los Angeles County’s health officer told Healthline.
And in mid-September, President Joe Biden announced that all employers with more than 100 workers must require their employees to either be vaccinated or tested for COVID-19 on a weekly basis. This affects nearly 80 million people in the United States.
In addition, all workers at healthcare facilities that receive federal Medicare or Medicaid funds, as well as all employees and contractors of the federal government, must be vaccinated.
The view from the unvaccinated
Those choosing to remain unvaccinated say all these limitations can make a person feel isolated and singled out.
“This is where we are headed,” Ohio resident Renee Denton, who has no plans to get vaccinated, told Healthline.
Susan, who preferred not to use her full name due to the pushback she’s received, works in the public health industry and decided not to get vaccinated, because she had a mild case of COVID-19 and feels she now has natural immunity.
Susan said these restrictions make unvaccinated people feel targeted as well as misunderstood.
“I’m not anti-vax. I just want to take it when I think I need it,” Susan said.
She remembers watching with concern when President Biden announced the workplace vaccine requirements on national television last month.
“I just feel like a target who is being bullied by someone who was [supposed] to bring an end to this pandemic and protect me,” she said.
Since she has small children and doesn’t attend events outside her home often, Susan said she’s not that concerned — for now — about restrictions. But she does project ahead and wonder.
“I guess the one thing would be that I think some cultural institutions that I might want my kids to experience might not allow us in — like orchestra hall, museums, theatrical productions,” she said.
It also could mean changes in how they choose vacations.
“My husband and I would like to take a short vacation, and we thought about a weekend in New York City, but are not going to do that now. We will probably go to Key West or something instead,” she said.
For Denton, a big impact will be dining out, something she loves to do.
The same goes for planning their annual family vacations. Now, Denton said, they will cherry-pick spots that are more open to the unvaccinated and within driving distance, since they might face flying restrictions.
“Eventually,” she said, “we could end up in a situation where we can never fly again.”
Her employer has said they’ll be requiring vaccinations for all employees, even though Denton works from home for now.
Denton said, because she traveled before the pandemic once or twice per year, she’d have to vaccinate to keep her job.
She’s waiting and hoping for a religious exemption to come. Otherwise, she said, she could be out of a job.
Susan is weighing whether she will quit her job or get vaccinated when vaccine mandates arrive. She’s leaning toward quitting.
She believes the restrictions now being implemented at the workplace, businesses, and entertainment venues are too severe.
“There are people like me who have been completely ostracized,” the Minnesota resident said. “It’s become so political. People want to put you in a camp. They hear you’re unvaccinated and they automatically assume you’re [a right wing Republican]. Well, that’s not me.”
Denton wonders if vaccinations will even help get the world out of the pandemic.
“It’s just going to create division, that’s all,” she said. “I think anyone who wants to be vaccinated is at this point.”
Personalizing health
Experts grapple with the need to protect the fragile and young but also point out that, while it may be infuriating to some, everyone who is unvaccinated doesn’t hold identical beliefs.
They also note that recent history may have helped push the United States toward this moment.
Jennifer Reich, PhD, is a professor of sociology at the University of Colorado at Denver and the author of “Calling the Shots: Why Parents Reject Vaccines.”
Reich sees part of the divide as historical, driven by the nation’s push for personal healthcare responsibility that came in full swing during the 1980s.
“When you put it in historical context and ask what is the boundary between community responsibility and personal freedom, you can see some interesting things,” Reich told Healthline.
Health, she pointed out, has become very much a personal responsibility. Jogging was a first push toward it. So were things like tracking your own BMI and weight.
There’s even a booming industry around it: fitness trackers are plentiful and seem to be on the wrist of just about everyone you pass now. Many closely count how many steps they’ve taken in a day.
To a point, it has worked in helping people embrace healthier living. But, Reich said, it has also heightened the feeling of personal choice around medicine, something people might not have seen in other vaccination eras, such as the emergence of the polio vaccine in the 1950s.
“You have to sympathize with this,” Reich said, “because we have totally individualized the responsibilities of health.”
The challenge with that, she noted, is “public health [as a whole] sold personal responsibility, not community good. [People who are choosing not to vaccinate for personal reasons] are not making that up. We sold it.”
Now, she said, with a highly infectious disease at play, that personal focus does not work.
When the polio vaccine first arrived, she said, vaccinations for children were not mandated at first. So, wealthier and more connected families got access quickly. Those with less did not.
So, Reich said, mandates were put in place — with federal funding — to even the field. It worked.
But this pandemic, she said, is the first time in U.S. history that adults are being asked to take part in a community solution and are being pushed to do so via restrictions.
“Clearly, we don’t have a culture set up for this,” she said.
Speaking to the unvaccinated
Dr. Mary Tipton is on the front line of patient care. With a busy practice in Utah, she treats thousands of people. Her goal is for every one of her patients who don’t have medical restrictions to get the COVID-19 vaccine.
But she feels restrictions are the wrong move.
“The risk I see with running with mandates is they become even more in opposition,” Tipton told Healthline. “When you push something on someone like this, they push back. They think, ‘I may as well take a stand,’ and they dig their heels in.”
Tipton believes a personal one-on-one approach works best and can come from a trusted source, such as a medical professional.
She recently spoke with about 150 Air Force members. Many, she said, are upset at the notion that they may be forced to take the vaccine or lose their positions.
“They are really good people and when you sit down with them, you’ll see they’ve put great thought into this,” she said.
They told her they feel the public sees them as ignorant, something that is hurtful and wrong in their point of view.
And soon, she said, they’ll feel ostracized in the most visible way by losing their jobs.
Her hope? That more unvaccinated people find a chance to speak with someone they trust and weigh what they think with what they may learn.
Will it work? Tipton isn’t sure. She noted that, should workplace vaccine requirements come to her area, she may lose employees over it.
“I don’t think this is a high yielding policy,” she said.
Where to go from here
Mandates are not going away, according to those overseeing them.
While Los Angeles County has imposed among the most restrictive rules, they are not adverse to the idea of placing even stricter rules should the need arise.
“We will continue to monitor the situation as we move into the winter months and hope no additional requirements will be needed,” Davis said.
“But, if they are, we [in Los Angeles] county must use every available tool to prevent the spread of COVID-19 and to continue to save lives in the months ahead, while also keeping schools open and safe and protecting our economy from damage,” he added.
That means, said Carpiano, society will have some adjusting to do.
“No matter how optimal a policy is, it’s not going to be [well-received] by everyone,” he said. “That’s reality.”
Also reality, he said, is the fact that people are dying.
“The fact is, we are in a major crisis,” he said. “COVID is the number three cause of death now and we’re not getting out of it easily. This is going to be our new reality. That’s the hard truth of it.”
And while Carpiano feels for those like Susan, he said, he hopes people realize the power of greater good.
Even work mandates, Carpiano said, fit that “greater good” need.
“Those who say [a vaccine mandate for work] is overstepping? I say it is showing employees that their health and safety is important. Isn’t that why unions were formed?” he said.
Jamie West, a resident of South Dakota who is waiting with hope on a religious exemption, told Healthline she sees this as a “fight for freedom.”
“A last stand of sorts. If we can’t hold onto this freedom of sovereignty of ourselves, what will we have left?,” she said.
Learning from all this
Carpiano hopes that sociologists and society at large study this pandemic, learn from it, and push for change.
First up, he said, is looking at the spread of misinformation via social media that he believes impacted peoples’ decisions.
“Social media is a bit of the Wild West,” he said. “The extent to which misinformation can undermine public health decisions is one we need to look closely at.”
He also hopes we look at federalism versus local action, and how the country can better respond to things, such as a pandemic.
“A hurricane is one thing,” Carpiano said. “It’s regionalized. It’s a clear situation, and we can take action. But when something hits the entire nation like this and in unique ways in different parts? We have to learn how to respond as a whole to something that looks different in many places.”
We also have to figure out what motivates people.
“We tried,” he said. “And even after seeing loved ones die, people still decided not to get vaccinated. I’m not sure what motivation we can find beyond that.”
Reich hopes more people come to the conclusion to get vaccinated.
“With freedom comes responsibility,” she said. “That’s the reality.”
* This article was originally published here
Friday, September 24, 2021
Nursing Home Staff Closest to Patients Are Least Likely to Get COVID Vaccines
Category: Health News
Created: 7/30/2021 12:00:00 AM
Last Editorial Review: 7/30/2021 12:00:00 AM
* This article was originally published here
Thursday, September 23, 2021
Wednesday, September 22, 2021
Seniors Rarely Discuss Their Drinking With Their Doctors
Category: Health News
Created: 7/30/2021 12:00:00 AM
Last Editorial Review: 7/30/2021 12:00:00 AM
* This article was originally published here
Tuesday, September 21, 2021
Depression spiked for Black Americans after George Floyd’s murder
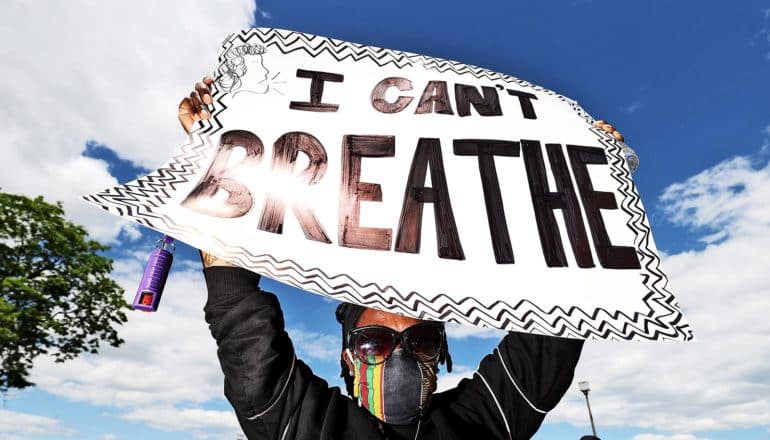
A new study shows just how much of a psychological toll the murder of George Floyd took on people in America, particularly among Black Americans.
Following the murder of Floyd, an unarmed Black man killed by a white police officer, more than one-third of Americans reported feelings of anger and sadness in the week after his death.
Black Americans experienced grief at a much higher rate: Nearly one-half of all Black Americans reported feeling angry or sad in the wake of Floyd’s death, and nearly one million more Black Americans screened positive for depression, according to a new analysis of US Gallup and census data.
“People realize ‘that could have been me or a member of my family.’ It touches the emotional core of who we are.”
“Coming out of the COVID-19 crisis, national surveys were tracking how the mental health of the population was developing. When George Floyd was murdered, these data collections caught the dramatic psychological impact, giving us a glimpse of how this collective moral injury impacted emotions and mental health,” says Johannes Eichstaedt, an assistant professor (research) of psychology at Stanford University and lead author of the new paper in the Proceedings of the National Academy of Sciences.
In the weeks after Floyd’s murder on May 25, 2020, protests erupted across the country after millions of people watched the chilling video footage of his murder. His violent death, along with the deaths of Ahmaud Arbery, Breonna Taylor, and other victims of police brutality, galvanized a nationwide movement—the largest in the country’s history—about the many ways structural racism and bias is embedded in American lives.
“To see that movement manifested at the psychological level is powerful, showing that people were not only socially invested in change, but that they were emotionally invested as well,” says coauthor Steven O. Roberts, an assistant professor of psychology.
Anger and sadness
To examine the rates of anger and sadness following Floyd’s murder, researchers used the Gallup COVID-19 Panel survey from four weeks before and after his death.
Data showed that immediately after Floyd’s death, feelings of anger increased by about half in the population: Roughly 38% of Americans said they experienced anger. Sadness increased about a third, with 38% also reporting feelings of loss, despair, and grief.
Feelings of anger and sadness were particularly acute in the Black community in the wake of Floyd’s death.
“In order to have a more equitable society in which Black Lives Matter, we must acknowledge that the mental lives of Black Americans matter as well.”
Nearly 1 in 2 Black Americans reported feelings of anger (48%), representing a 2.1-fold increase from the week before. Sadness also soared to 47% of Black Americans reporting feelings of loss, despair, and grief. Among white Americans it was about 1 in 3: Some 34% said they experienced anger and 36% sadness.
“Seeing a member of one’s group killed engenders a feeling of threat and vulnerability,” says Eichstaedt, who also directs Stanford’s Computational Psychology and Well-Being Lab. “People realize ‘that could have been me or a member of my family.’ It touches the emotional core of who we are.”
These spikes are the largest Gallup has observed since 2009, when the public opinion firm began tracking emotions, the researchers say.
“Data from a representative Gallup survey of Americans suggest that anger and sadness in the US population increased to unprecedented levels after his death,” they wrote in the paper. While Gallup did not consistently measure anger and sadness during the previous decade, the highest levels of anger and sadness previously recorded occurred after the Sandy Hook Elementary School shooting, with 16% reporting feelings of anger and 22% sadness—less than after Floyd’s death reported here.
The researchers also found that when compared to other states, depression and anxiety were higher in Minneapolis, Minnesota, where Floyd’s murder occurred. This finding is consistent with previous scholarship that showed that location matters: the traumatic impact of racial violence and police brutality is larger in the communities in which they occur.
‘Racism gets under the skin, literally’
The researchers also wanted to examine how people’s mental health may have suffered. During the pandemic, rates of depression and anxiety had increased in the population—but the murder of George Floyd added additional mental health burden, particularly for Black Americans, the researchers found.
In their analysis of US Census Household Pulse data gathered in the five weeks before and the week after Floyd’s death, the researchers found that among Black Americans, depression increased 3.2%: 26.7% to 29.9%. For white Americans, it increased 1.2%.
The researchers estimate that for Black Americans, this 2% difference in increase is equivalent to an additional 900,000 individuals screening positive for depression. The researchers estimate that these additional depression screens are each associated with three to seven days of mental unhealth, thus translating to between 2.7 and 6.3 million additional mentally unhealthy days among Black Americans.
For the researchers , the racial disparities revealed in these data show the disproportionate burden that witnessing police violence bears on the Black community.
Previous research has shown that police killings of unarmed Black Americans can be a vicariously traumatizing experience for other Black Americans. Eichstaedt and Roberts’ study confirms the unevenness those spillover effects have in American society.
“Racism gets under the skin, literally,” says Roberts, who also directs the Social Concepts Lab at Stanford. “Not only are Black Americans at increased risk of encountering racial discrimination in the real world—including police brutality—they are also at increased risk of carrying around the psychological burden of that unfortunate reality.”
That psychological burden can often translate into physical ones. Trauma has been shown to have damaging effects on people’s physical health, including an increased risk of heart disease, high blood pressure, diabetes, and obesity, among other effects, the researchers note in the paper.
“In order to have a more equitable society in which Black Lives Matter, we must acknowledge that the mental lives of Black Americans matter as well,” the scholars write.
The death of George Floyd also occurred during the COVID-19 pandemic that saw Black and brown communities shouldering a disproportionate burden of the disease. Floyd’s death brought on a new level of fatigue, Roberts says.
“We need to understand and appreciate that Black Americans—in addition to dealing with the pandemic and work and family responsibilities—have had to carry the weight of George Floyd’s murder,” he says. “Being a Black American necessitates strength and perseverance, and that was especially true in 2020.”
Additional coauthors are from the University of Pennsylvania and Stanford.
Source: Stanford University
The post Depression spiked for Black Americans after George Floyd’s murder appeared first on Futurity.
* This article was originally published here
Monday, September 20, 2021
Turning 65 Brings Big Health Care Cost Savings, Study Finds
Category: Health News
Created: 9/15/2021 12:00:00 AM
Last Editorial Review: 9/15/2021 12:00:00 AM
* This article was originally published here
Sunday, September 19, 2021
COVID patients face risk for self-attacking antibodies

A new study shows that at least 1 in 5 hospitalized COVID-19 patients develops antibodies that attack their own tissue within a week of admission.
Autoantibodies are antibodies directed at their own tissues or at substances immune cells secrete into the blood. Autoantibodies can be early harbingers of full-blown autoimmune disease.
“If you get sick enough from COVID-19 to end up in the hospital, you may not be out of the woods even after you recover,” says PJ Utz, professor of immunology and rheumatology at Stanford Medicine.
As reported in Nature Communications, researchers looked for autoantibodies in blood samples drawn during March and April of 2020 from 147 COVID-19 patients at three university-affiliated hospitals: Philipps University Marburg in Germany, the University of Pennsylvania, and Stanford, and from a cohort of 48 patients at Kaiser Permanente in California. They used blood samples drawn from other donors prior to the COVID-19 pandemic as controls.
The researchers identified and measured levels of antibodies targeting the virus; autoantibodies; and antibodies directed against cytokines, proteins that immune cells secrete to communicate with one another and coordinate their overall strategy.
Upward of 60% of all hospitalized COVID-19 patients, compared with about 15% of healthy controls, carried anti-cytokine antibodies, the researchers found. This could be the result of immune-system overdrive triggered by a virulent, lingering infection. In the fog of war, the abundance of cytokines may trip off the erroneous production of antibodies targeting them, Utz says.
If any of these antibodies block a cytokine’s ability to bind to its appropriate receptor, the intended recipient immune cell may not get activated. That, in turn, might buy the virus more time to replicate and lead to a much worse outcome.
On the hunt for autoantibodies
For about 50 patients, blood samples drawn on different days, including the day they were first admitted, were available. This allowed the researchers to track the development of the autoantibodies.
“Within a week after checking in at the hospital, about 20% of these patients had developed new antibodies to their own tissues that weren’t there the day they were admitted,” Utz says. “In many cases, these autoantibody levels were similar to what you’d see in a diagnosed autoimmune disease.”
In some cases, the presence of those newly detected autoantibodies may reflect an increase, driven by the immune response, of antibodies that had been flying under the radar at low levels, Utz says. It could be that inflammatory shock to the systems of patients with severe COVID-19 caused a jump in previously undetectable, and perhaps harmless, levels of autoantibodies these individuals may have been carrying prior to infection.
In other cases, autoantibody generation could result from exposure to viral materials that resemble our own proteins, Utz says.
“It’s possible that, in the course of a poorly controlled SARS-CoV-2 infection—in which the virus hangs around for too long while an intensifying immune response continues to break viral particles into pieces—the immune system sees bits and pieces of the virus that it hadn’t previously seen,” he says. “If any of these viral pieces too closely resemble one of our own proteins, this could trigger autoantibody production.”
Another reason to get the vaccine
The finding bolsters the argument for vaccination, he adds. Vaccines for COVID-19 contain only a single protein—SARS-CoV-2’s so-called spike protein—or the genetic instructions for producing it. With vaccination, the immune system is never exposed to—and potentially confused by—the numerous other novel viral proteins generated during infection.
In addition, vaccination is less intensely inflammatory than an actual infection, Utz says, so there’s less likelihood that the immune system would be confused into generating antibodies to its own signaling proteins or to the body’s own tissues.
“Patients who, in response to vaccination, quickly mount appropriate antibody responses to the viral spike protein should be less likely to develop autoantibodies,” he says.
Indeed, a recent study in Nature to which Utz contributed showed that, unlike SARS-CoV-2 infection, the Pfizer COVID-19 vaccine doesn’t trigger any detectable generation of autoantibodies among recipients.
“If you haven’t been vaccinated and are telling yourself, ‘Most people who get COVID get over it and are OK,’ remember that you can’t know in advance that when you get COVID-19 it will be a mild case,” Utz says.
“If you do get a bad case, you could be setting yourself up for a lifetime of trouble because the virus may trip off autoimmunity. We can’t say yet that you’ll definitely get an autoimmune disease—we haven’t studied any patients long enough to know whether these autoantibodies are still there a year or two later, although we hope to study this—but you certainly might. I wouldn’t want to take that chance.”
Utz intends to study blood samples from SARS-CoV-2-infected people who are asymptomatic or who’ve had mild COVID-19 symptoms. That could help determine whether the massive hyperactivation of the immune system, which doesn’t occur in mildly symptomatic or asymptomatic people, is what causes trouble, or whether the mere molecular resemblance of SARS-CoV-2 proteins is enough to trigger autoantibody generation.
Additional coauthors are from the University of Pennsylvania, Philipps Marburg University, the University of Tennessee, Oklahoma Medical Research Foundation, Kaiser Permanente Northern California, and Stanford.
Funding for the study came from the National Institutes of Health, the Henry Gustav Floren Trust, the Parker Institute for Cancer Immunotherapy, the Sean N. Parker Center, the Frank Quattrone and Denise Foderaro Family Research Fund, the Chan Zuckerberg Biohub, the Allen Institute for Immunology, the CEND COVID Catalyst Fund, the Chen Family Research Fund, the Carreras Foundation, the Foundation for Pathobiochemistry and Molecular Diagnostics, Universities Giessen and Marburg Lung Center, the German Center for Lung Research, the Deutsche Forschungsgemeinschaft, and Stanford Medicine.
Source: Stanford University
The post COVID patients face risk for self-attacking antibodies appeared first on Futurity.
* This article was originally published here
Saturday, September 18, 2021
EXPLAINER: What are 'Crisis Standards of Care?'

As the spread of the delta variant continues unabated in much of the U.S., public health leaders have approved health care rationing in Idaho and parts of Alaska and Montana.
* This article was originally published here
Friday, September 17, 2021
After an ICU Stay, Social Support Crucial for Seniors' Survival
Category: Health News
Created: 9/15/2021 12:00:00 AM
Last Editorial Review: 9/15/2021 12:00:00 AM
* This article was originally published here
Thursday, September 16, 2021
New rule for teen drivers at night cut crashes and deaths

New research finds that a ban on new drivers carrying multiple passengers at night more than halved crashes, casualties, and deaths.
In most countries, traffic accidents are the leading cause of death for teenagers, with risky driving accounting for a large fraction of those deaths.
Many governments have implemented driving restrictions to reduce risks among teens, with varying degrees of success.
The new National Bureau of Economic Research working paper examines the effects of a ban on carrying multiple passengers between 11 PM and 4:59 AM for first-year drivers under the age of 21.
Tim Moore, an associate professor of economics at the Krannert School of Management and a Purdue University Research Center in Economics faculty affiliate, and coauthor Todd Morris of the Max Planck Institute for Social Law and Social Policy estimate that the restriction reduced reported hospitalizations and fatalities by 58%, with 41 fewer hospitalizations, 98 fewer minor injuries, and 164 fewer crashes with property damage per 100,000 first-year drivers.
The ban, implemented in July 2007 in the Australian state of New South Wales, is shown to be as effective as harsher restrictions that tend to discourage teens from getting licenses and starting to drive.
“Delaying when teens can start driving also delays driving experience and the benefits of driving independently,” Moore says.
His study finds no evidence that the New South Wales restriction delays the development of driving skills, probably because it targets a very specific type of driving.
The ban also seems to have had persistent effects on driving behavior, unlike some other restrictions.
“We find significant reductions in nighttime multipassenger crashes in the second and third years of driving,” Moore says. “We see no differences beyond the third year, but by that time teens have become much safer drivers—their crash rates are one-fifth those of first-year drivers.”
Timing is important: The safety effects are more persistent among teens always subject to the restriction versus those who started driving before the restriction went into effect.
This paper adds to the literature on teen driving, which shows that while some restrictions reduce accidents, few lead to persistent behavioral changes. For example, speed-monitoring campaigns do not reduce accidents once they end, and ongoing cellphone texting bans decrease crashes for a month or two before returning to their original levels.
The findings by Moore and Morris suggest targeted policies that place limited restrictions on teens’ driving behavior, especially when implemented at the right time, can both improve safety and allow teens to develop driving skills.
Source: Purdue University
The post New rule for teen drivers at night cut crashes and deaths appeared first on Futurity.
* This article was originally published here
Wednesday, September 15, 2021
Is a combo COVID/flu shot on the way?

During the next few weeks or months, you might find yourself dropping by the doctor's office or pharmacy to get your annual flu shot along with a dose of COVID vaccine.
* This article was originally published here
Tuesday, September 14, 2021
Changes to workplace cafeteria menus nudge workers to consume fewer calories

A study carried out at 19 workplace cafeterias has shown that reducing portion sizes and replacing higher calorie food and drinks with lower calorie options led to workers buying food and drink with fewer calories.
* This article was originally published here
Monday, September 13, 2021
Skin healing gene tweaks may play a role in diabetic wounds

Researchers have uncovered a new mechanism that promotes wound healing in skin.
The molecular pathway identified is controlled by an evolutionary conserved gene called a Grainyhead like 3 (GRHL3), which is a gene required for mammalian development. Without this gene, several abnormalities may occur, including spina bifida, defective epidermal barrier, defective eyelid closure, and soft-tissue syndactyly, a condition in which children are born with fused or webbed fingers.
The study reveals how during wound healing, GRHL3 works to activate a protein coding gene called Fascin Actin-Bundling Protein 1 (Fscn1), to loosen the adhesion between wounded skin cells so they can migrate efficiently to close the wound.
Researchers also found that alterations in this process may result in chronic, non-healing wounds, such as diabetic ulcers that affect millions of patients every year.
“What’s exciting about our findings is that we have identified a molecular pathway that is activated in normal acute wounds in humans, and altered in diabetic wounds in mice,” says Ghaidaa Kashgari, a postdoctoral researcher in the University of California, Irvine, School of Medicine Department of Medicine. “This finding strongly indicates clinical relevance and may improve our understanding of wound healing biology and could lead to new therapies.”
Acute skin wound healing progresses through four overlapping phases: hemostasis, inflammation, proliferation, and tissue remodeling. Although wounds close partially by dermal contraction, reepithelialization occurring during the proliferation phase, is a key step in wound healing.
During reepithelialization, keratinocytes, which are cells that make up the outermost layers of the skin, migrate on top of the underlying granulation tissue, which is the lumpy, pink tissue that forms around the edges of a wound. Ultimately, the keratinocytes meet migrating keratinocytes from the opposing margin to close the wound.
“Despite significant advances in treatment, much remains to be understood about the molecular mechanisms involved in normal wound healing,” says senior author Bogi Andersen, a professor in the Departments of Biological Chemistry and Medicine at the UCI School of Medicine.
“Our findings uncover how abnormalities in the GRHL3/FSCN1/E-cadherin pathway could play a role in non-healing wounds which needs to be further investigated.”
The research appears in JCI Insight.
Support for this work came from the National Institutes of Health and the Irving Weinstein Foundation.
Source: UC Irvine
The post Skin healing gene tweaks may play a role in diabetic wounds appeared first on Futurity.
* This article was originally published here
Sunday, September 12, 2021
What are the ethics of getting a COVID-19 vaccine booster?

After the Biden administration’s announcement on COVID-19 booster shots, questions came up about the ethics of vaccinated people in the US getting a booster when so many people around the world are still waiting for their first dose.
And while we’re pondering ethics, is there a selfish argument for the US to lead efforts to vaccinate people around the world? What about vaccine mandates? And when will we be able to vaccinate kids?
Here, Julie Swann, professor of industrial and systems engineering, and Matt Koci, a virologist and immunologist and professor in the poultry science department, both at North Carolina State University, weigh in on these questions and more:
The post What are the ethics of getting a COVID-19 vaccine booster? appeared first on Futurity.
* This article was originally published here
Saturday, September 11, 2021
Friday, September 10, 2021
White House Reverses Policy Limiting U.S. Nursing Home Fines
Category: Health News
Created: 7/30/2021 12:00:00 AM
Last Editorial Review: 7/30/2021 12:00:00 AM
* This article was originally published here
Thursday, September 9, 2021
Wednesday, September 8, 2021
Black and Mexican American adults develop diabetes at a younger age

Certain racial and ethnic minorities develop type 2 diabetes at a younger age than white Americans, meaning current diabetes screening and prevention practices for them may be inadequate and inequitable, reports a new Northwestern Medicine study.
* This article was originally published here
Tuesday, September 7, 2021
Nursing homes are ground zero for COVID reinfections

New research sheds light on why COVID-19 has hit nursing homes so hard.
Residents in long-term care facilities had a significantly higher rate of reinfection than people in the general population, according to a new study.
The study in the journal The Lancet Regional Health–Americas analyzed nine months of testing data, just prior to the roll-out of vaccines in long-term care facilities, a period that allowed researchers to look at test results in the setting of natural exposure to the virus.
They identified that 2.6% of residents in Connecticut’s 212 nursing homes had one or more repeat positive SARS-CoV-2 PCR tests occurring as early as 90 days after an initial positive test. This percentage was significantly higher than other demographics, such as younger adults, or community-dwelling elderly.
Even more concerning, 12.6% of the elderly with a second positive test after 90 days died shortly after that repeat positive test. While genetic sequencing was not available, several lines of evidence supported that re-infection may have been responsible for the repeat positive tests, including the fact that 80% of those elderly had an intervening negative test.
“While nursing home residents represent some of the most elderly and frail individuals in our community, we were still quite surprised at the patterns of test results and the outcomes. This was an early clue as to the less robust and waning immunity that may be seen in this vulnerable population following natural SARS-CoV-2 infection,” says Sunil Parikh, associate professor at the Yale University School of Public Health and the study’s lead author.
A critical tool to contain outbreaks in nursing homes has been the use of surveillance testing for the SARS-CoV-2 virus. While tests were hard to come by in the early months of the pandemic, states such as Connecticut were able to conduct rapid and frequent comprehensive testing of nursing home residents by mid-May 2020. The sheer number of positive tests was sobering, but this allowed nursing homes, in collaboration with the Connecticut Department of Public Health (CT DPH) and the Yale School of Public Health to identify outbreaks, analyze data, and separate individuals who were infected, thereby limiting these potentially explosive outbreaks.
It soon became clear, however, that the interpretation of tests was becoming complicated in such settings, as many individuals remained positive for extended periods of time, while some became positive again weeks or months after an initial infection. To help guide the community, the Centers for Disease Control and Prevention provided guidelines suggesting that repeat testing was generally not warranted in the 90 days following initial positive test results.
As the frequency of repeat positive tests began to increase months into the pandemic, questions began to accumulate. Were these residents being re-infected so soon after an initial infection, were these false positive tests, or were these persisting infections?
To understand the landscape of testing results over time, researchers mapped results using the comprehensive surveillance system developed over the early months of the pandemic.
While the study was conducted prior to vaccine roll-out, the potentially short duration of protection following natural infection has implications for nursing homes that are now many months out of initial vaccination efforts. Together with the more transmissible Delta variant, gaps in staff vaccination coverage, and the need for boosters in these settings, this scenario should raise concern about a renewed risk of COVID-19 outbreaks in congregate settings.
Sadly, the fight is not over, and we must remain vigilant in monitoring infection rates in nursing homes and ensuring vaccination of all staff and residents, says coauthor Jillian Armstrong, a doctoral student at CT DPH.
Source: Yale University
The post Nursing homes are ground zero for COVID reinfections appeared first on Futurity.
* This article was originally published here
Monday, September 6, 2021
App-based self-test program improves HIV detection

A new app-based HIV self-test program not only successfully linked participants to counseling services and care, but also detected new infections and increased referrals to self-test.
In the shadow of the COVID-19 pandemic, HIV continues to be a major global public health issue, affecting an estimated 40 million people.
“Our study shows that a flexible, anonymized, secure, app-based digital program can be successfully deployed with young digitally savvy populations, even in low-resource settings.”
As COVID-19 disrupts health care systems, digital health initiatives like the new program are stepping in to fill the gap, offering the possibility to increase access to effective HIV prevention, diagnosis, treatment, and care.
Nitika Pant Pai at the Research Institute of the McGill University Health Centre (RI-MUHC) developed the self-test program, called HIVSmart!, and implemented it in township populations of Western Cape in South Africa with the collaboration of physicians at the University of Cape Town and community healthcare workers.
The findings, published in BMJ Global Health, compares the HIV self-test program to conventional HIV testing and suggests that self-testing strategies using innovative digital technologies that provide access to care could accelerate progress towards UNAIDS targets for HIV elimination worldwide.
Recent HIV self-test studies have shown increases in self-test uptake and detection of new HIV infections. However, without the appropriate programs and logistics, linking people to either preventative care (i.e., pre-exposure prophylaxis, partner notification, and medical circumcision) or treatment care has remained a challenge.
“The WHO has called for evidence for the use of digital supports and community-based health care workers to improve services associated with HIV self-testing,” explains Pant Pai, physician and scientist in the infectious diseases and immunity in global health program at the RI-MUHC and first author of the study.
“Our study shows that a flexible, anonymized, secure, app-based digital program can be successfully deployed with young digitally savvy populations, even in low-resource settings.”
“The advent of COVID-19 has reduced access to healthcare services. This, combined with the fact that more than half of new HIV infections in many African countries are in the young tech-savvy population (15 to 30-year age group), means that HIV self-testing with digital support tools will fill a huge unmet need and improve detection rates and links to care,” adds co-principal investigator Keertan Dheda, director of the Centre for Lung Infection and Immunity at University of Cape Town in South Africa and professor of mycobacteriology and global health at the London School of Hygiene and Tropical Medicine in the UK.
“HIV and AIDS affect millions worldwide, and knowing you have it can certainly help prevent its transmission. Dr. Pant Pai’s work is an essential step toward reducing and eliminating HIV transmission—one that will improve and save countless lives. I am grateful to our community of donors for supporting this important initiative,” says Julie Quenneville, president and CEO of the MUHC Foundation.
Grand Challenges Canada, the Medical Research Council South Africa Department of Science & Technology South Africa (government of South Africa), the MUHC Foundation, and OraSure funded the work.
Source: McGill University
The post App-based self-test program improves HIV detection appeared first on Futurity.
* This article was originally published here
Sunday, September 5, 2021
Just 250 Fewer Calories Per Day Brings Big Health Rewards for Obese Seniors
Category: Health News
Created: 8/2/2021 12:00:00 AM
Last Editorial Review: 8/2/2021 12:00:00 AM
* This article was originally published here
Saturday, September 4, 2021
Concussion recovery takes up to 28 days, not 14

The largest study of concussion ever conducted in college athletes redefines the timeline for recovery from the suggested normal recovery time of up to 14 days to up to 28 days.
“Normal return-to-play time was previously set at 14 days–meaning 50% of people recovered in that time. Our paper suggests that 28 days more fully encapsulates the recovery process. At that point, 85% of people have returned to play,” says Steve Broglio, director of the University of Michigan Concussion Center.
The study, which appears in the journal Sports Medicine, shows that though median recovery times were consistent with the previously suggested 14 days, it was not until one month post-injury that most athletes were cleared for unrestricted sport participation.
This doesn’t mean that universities must revise their return to play protocols. “The RTP protocols are driven by clinical presentation (symptoms), not time, so they don’t need to be revised,” Broglio says.
Rather, coaches, parents, and athletes should reframe their expectations for return to play, in part to avoid stigmatizing concussed athletes who take longer than 14 days to recover, he says.
Reframing the normal recovery time to 28 days helps eliminate unintentional social pressure from teammates, coaches, or parents who hope to see their player back on the field. If a concussed athlete takes longer than 14 days or up to a month, that’s completely normal, he says.
There wasn’t much variation in recovery times among study subgroups, with various factors altering recovery by only up to two days. The total return-to-play duration was shorter with ADHD medication usage, males, and greater assessment frequency. Those with greater initial post-injury symptom severity, practice/training-related injuries, and three or more prior concussions had longer recoveries.
Concussion management recommendations are outlined every four years by the Concussion in Sport Group, an international body that reviews the medical literature and develops guidelines on clinical care. This paper and others resulting from the CARE Consortium will likely be taken into consideration when the group meets next year, says Broglio, who is also a member of CISG.
Despite increased research in concussion over the previous decade, the trajectory of concussion recovery times across diverse populations of athletes has remained poorly defined, because most sport concussion research centered on male athletes in collision sports, or on female soccer players, Broglio says.
The current study included 34,709 male and female athletes from 30 colleges and universities—more than 1,700 of whom were concussed while participating in 22 sports.
Concussed male athletes most commonly played football (54.7%), soccer (10.7%), basketball (6.8%), and wrestling (6.4%), while concussed female athletes most commonly played soccer (23.4%), volleyball (14%), basketball (12.9%), and lacrosse (8.4%).
Male and female athletes took about the same amount of time to recover from concussion, give or take a day, Broglio says.
Concussion education and treatment has improved dramatically in the last two decades, he says.
“Back when I started in concussion research 20 years ago, we’d manage these injuries with a light switch. We’d ask, ‘Do you have symptoms?’ and if the answer was no, the athlete was put back on the field. Gone are the days when concussed athletes are put back in the same day,” Broglio says.
“Now, we can think of it as a dial, where we slowly progress people back into the sport. Once a player is asymptomatic, it can still take some time. We have to respect the injury and respect the recovery process.”
Additional coauthors are from Indiana University, the Medical College of Wisconsin, and CARE Consortium investigators.
Source: University of Michigan
The post Concussion recovery takes up to 28 days, not 14 appeared first on Futurity.
* This article was originally published here
Friday, September 3, 2021
Thursday, September 2, 2021
Glioblastoma drug for dogs may work for people

A treatment for glioblastoma in dogs has promising implications for the human version of the aggressive cancer that grows in the brain, according to a new study.
The study in Clinical Cancer Research describes the results of a Phase I clinical trial in which investigators tested a STING (STimulator of INterferon Genes) drug injected directly into the glioblastoma of five dogs that had previously been diagnosed with the cancer. Glioblastoma is the second-most common type of brain cancer in dogs.
STING agonists can induce immunological responses that allow the immune system to fight otherwise immunologically resistant cancer cells.
MRI scans taken over the course of the 10-month trial revealed that some of the dogs, even with a single dose, responded to the treatment with apparent reductions in their tumor volume, including one complete response in which the tumor appeared to completely disappear.
That led the researchers to conclude that this therapy can trigger a robust, innate anti-tumor immune response and may be highly effective on recalcitrant tumors such as glioblastoma.
“With this therapy, we were trying to take tumors that do not, on their own, generate a lot of immune response and turn them into tumors that do by injecting them with this immunotherapy agent,” says Beth Boudreau, an assistant professor of neurology at Texas A&M University.
This clinical trial was based on the team’s earlier research, which analyzed a massive canine genomic dataset collected from multiple glioma samples. The researchers found that canine and human gliomas are molecularly similar, suggesting that the two diseases have a similar mutational, cancer-causing process that would enable similar treatment strategies.
Both canine and human gliomas tend to have a poor prognosis, as they are difficult to surgically remove and traditional therapies come with multiple side effects and are expensive. Even after a high-risk surgery to remove the tumor and radiation therapy and/or chemotherapy, humans with glioblastoma may only survive a few more months.
“In the canine clinical trial, dogs did not receive surgery to remove their tumors, which limited the dose we could safely deliver,” Boudreau says. “In humans with glioblastoma, our STING agonist will be combined with surgery, which should improve its safety and efficacy. Further investigation and refinement would be needed to determine the role of this therapy in treating brain tumors in dogs.”
Because of the simple delivery of the STING agonist and the marked volume reduction of the tumor, the researchers also believe this strategy may provide a viable adjunct therapeutic approach for human glioma.
In the next phase of the project, the researchers are exploring using a similar approach in clinical trials of human glioma patients who have undergone a surgical debulking.
Michael A. Curran, an immunologist and founder of ImmunoGenesis, developed the immunotherapy drug. Additional coauthors are from Northwestern University and the Texas A&M College of Veterinary Medicine & Biomedical Sciences’ (CVMBS) Veterinary Medical Teaching Hospital (VMTH).
Source: Texas A&M University
The post Glioblastoma drug for dogs may work for people appeared first on Futurity.
* This article was originally published here
Wednesday, September 1, 2021
Could a TB Vaccine Protect the Elderly From Severe COVID?
Category: Health News
Created: 8/5/2021 12:00:00 AM
Last Editorial Review: 8/5/2021 12:00:00 AM
* This article was originally published here